What is Morton’s Neuroma?
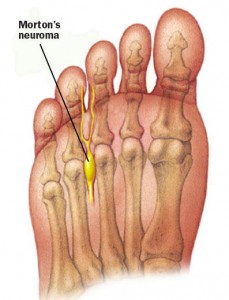
Morton’s Neuroma is a condition frequently seen at the San Diego Running Institute. It is often misdiagnosed or confused with plantar fasciitis or Metatarsalgia. Morton’s Neuroma occurs when the metatarsal bones become misaligned and squeeze the nerve, causing pain or numbness.
Morton’s Neuroma Symptoms
This condition causes shooting, burning, or electric-like pain, usually in the 2nd-4th toe. People will complain of pain in the ball of their foot, usually just behind the second or third toe that either causes numbness into the toes or shooting pain into the toes. The pain can be intense or just a dull ache that they describe but usually gets progressively worse with activity. The pain can be bad enough to cause you to stop running, and may even result in a limp.
How Do I Fix Morton’s Neuroma?
When the metatarsal bones are misaligned, they put pressure on the nerve. The pressure can be alleviated by aligning the bones properly so they aren’t squeezing the nerve. The San Diego Running Institute accomplishes this by using expertly made custom orthotics.
Incorrect Placement of Metatarsal Pads
Often, runners have been to a foot doctor or sports doctor who made them custom sports orthotics with a metatarsal pad (also known as a neuroma pad). When I ask the runner if it helps they will typically reply “no” and that “it does not help at all and may be making it worse”. The problem is that the metatarsal pad has been placed incorrectly on the custom orthotic. It is essential to have the metatarsal pad in the correct location in order to ease the condition. If you have custom orthotics that are not working or are uncomfortable San Diego Running Institute can fix them for you. Call us at 858-268-8525 or text 858-322-8581 to schedule an appointment. Within a week can can have your orthotics modified and helping to alleviate your Morton’s Neuroma.
Correct Placement of Metatarsal Pads
The nerve between the 2nd and 3rd metatarsals is inflamed due to narrowing of the space between them. This irritates the nerve which then causes the shooting pain and/or numbness into the toes. When the metatarsal pad is placed correctly just behind the metatarsal heads (just behind the painful location) alleviation of the foot and toe pain is achieved. It is not unusual for me to correctly place a metatarsal pad for a patient and have them walk pain free right then and there! If you have custom orthotics that are not working or are uncomfortable San Diego Running Institute can fix them for you. Call us at 858-268-8525 or text 858-322-8581 to schedule an appointment. Within a week can can have your orthotics modified and helping to alleviate your Morton’s Neuroma.
Custom Orthotics for Morton’s Neuroma
SDRI’s treatment usually begin with Superfeet orthotic inserts, then precisely placed pads in the correct location needed for healing and pain relief. There are many different metatarsal pads available but I have found our custom made foam met pads, most convenient and effective metatarsal pads to use for Morton’s Neuroma. While this is a fast and effective treatment for Morton’s Neuroma it is sometimes not enough to fix this common foot injury. We have also found that shoes with a wide toe-box can be complimentary to the placement of metatarsal pads. Some shoe brands such as Altra come with a naturally wide toe-box and a heel to toe ration of “0” which helps take pressure off the Morton’s Neuroma. If you live in San Diego Milestone Running Shop can help fit you for the proper Altra shoe.
How SDRI Can Help
The San Diego Running Institute can refer you to Dr. Bruce B. Allen D.C.. He has helped many runners and non-runners with Morton’s Neuroma and other foot pain conditions. If you have pain in the ball of your foot or have been diagnosed with Plantar Fasciitis, Morton’s Neuroma or Metatarsalgia and have not been helped call to schedule an appointment with Dr. Allen D.C. by calling (858) 268-8525 or text 858-322-8581
Medical Journal Articles About Mortons Neuroma & Related Conditions
[contentbox class=”contentbox3″]
Forefoot pain is one of the most common presenting problems in a foot and ankle practice. One of the most common presenting problems, yet most commonly missed problems, is a plantar plate tear. Often the problem is considered to be potential neuroma, fat pad atrophy, or a generalized diagnosis of metatarsalgia or metatarsal head overload. Unfortunately, not enough attention is placed on the plantar and medial/lateral ligamentous structures of the metatarsal-phalangeal joints. This lack of attention results in poor diagnosis, lack of care, treatment for the wrong condition, and ultimate frustration for the patients and doctor. “Plantar plate tears: a review of the modified flexor tendon transfer repair for stabilization.”– Originally Published by National Library of Medicine (NLM) in Jan, 2011.
[/contentbox]
[contentbox class=”contentbox2″]
OBJECTIVES:To determine the optimum position of a metatarsal (MT) pad to treat metatarsalgia. DESIGN:
We used a sensing mat with 16 x 16 sensors, 4.4 x 4.4 mm each, to measure plantar pressure in ten metatarsalgia patients walking with an MT pad in various positions. Peak pressures of the MT head and MT pad were analyzed. RESULTS:
Walking without MT pads, the peak pressure of the MT head was 678 +/- 227 and 687 +/- 228 kPa in one proximal and one distal row of three sensors. Placement of the MT pad resulting in peak pressure two sensors proximal to the peak pressure of the MT head did not significantly reduce peak pressure on the MT head. In contrast, placement of the MT pad resulting in peak pressure just proximal to the peak pressures of the MT head reduced the proximal and distal peak pressures on the MT head to 427 +/- 97 and 431 +/- 92 kPa (P < 0.05). CONCLUSIONS:
Optimum pressure reduction on the MT head is attained when the peak pressure generated by the MT pad is just proximal to the MT head. “Optimum position of metatarsal pad in metatarsalgia for pressure relief.” – Originally Published by National Library of Medicine (NLM) in July, 2005.
[/contentbox]
[contentbox class=”contentbox3″]
OBJECTIVE:The purpose of this study is to update a systematic review on manipulative therapy (MT) for lower extremity conditions. METHODS:
A review of literature was conducted using MEDLINE, MANTIS, Science Direct, Index to Chiropractic Literature, and PEDro from March 2008 to May 2011. Inclusion criteria required peripheral diagnosis and MT with or without adjunctive care. Clinical trials were assessed for quality using a modified Scottish Intercollegiate Guidelines Network (SIGN) ranking system. RESULTS:
In addition to the citations used in a 2009 systematic review, an additional 399 new citations were accessed: 175 citations in Medline, 30 citations in MANTIS, 98 through Science Direct, 54 from Index to Chiropractic Literature, and 42 from the PEDro database. Forty-eight clinical trials were assessed for quality. CONCLUSIONS:
Regarding MT for common lower extremity disorders, there is a level of B (fair evidence) for short-term and C (limited evidence) for long-term treatment of hip osteoarthritis. There is a level of B for short-term and C for long-term treatment of knee osteoarthritis, patellofemoral pain syndrome, and ankle inversion sprain. There is a level of B for short-term treatment of plantar fasciitis but C for short-term treatment of metatarsalgia and hallux limitus/rigidus and for loss of foot and/or ankle proprioception and balance. Finally, there is a level of I (insufficient evidence) for treatment of hallux abducto valgus. Further research is needed on MT as a treatment of lower extremity conditions, specifically larger trials with improved methodology. “Manipulative therapy for lower extremity conditions: update of a literature review.”
– Originally Published by National Library of Medicine (NLM) in Feb, 2012.
[/contentbox]
[contentbox class=”contentbox2″]
BACKGROUND:
Metatarsalgia is related to repetitive high-pressure loading under the metatarsal head (MH) that causes pain. The high pressure under the MH can be reduced by adequately applying metatarsal pads (MPs). Plantar pressure measurements may provide a method to objectively evaluate pressure loading under the MH. However, it is still unclear if the decrease in plantar pressure under the MH after MP treatment is associated with subjective improvement. This study aims to explore the correlations between subjective pain improvement and outcome rating, and the plantar pressure parameters in metatarsalgia patients treated using MPs.
METHODS:
Thirteen patients (a total of 18 feet) with secondary metatarsalgia were included in this study. Teardrop-shaped MPs made of polyurethane foam were applied just proximal to the second MH by an experienced physiatrist. Insole plantar pressure was measured under the second MH before and after MP application. Visual analog scale (VAS) scores of pain were obtained from all subjects before and after 2 weeks of MP treatment. The subjects rated using four-point subjective outcome scales. The Wilcoxon signed-rank test was used to analyze the difference between the plantar pressure parameters and VAS scores before and after treatment. The Kruskal-Wallis test was applied to compare the plantar pressure parameters in each outcome group. Pearson’s correlation was applied to analyze the correlation between the changes in plantar pressure parameters and VAS scores. Statistical significance was set as p < 0.05.
RESULTS:
MP application decreased the maximal peak pressure (MPP) and pressure-time integral (PTI) under the second MH and also statistically improved subjective pain scores. However, neither the pre-treatment values of the MPP and PTI shift in the position of the MPP after treatment, nor the age, gender and body mass index (BMI) of the subjects were statistically correlated with subjective improvement. Declines in the PTI and MPP values after MP application were statistically correlated with the improvement in VAS scores (r = 0.77, R2 = 0.59, p < 0.001; r = 0.60, R2 = 0.36, p = 0.009).
CONCLUSION:
We found that the successful decline in the PTI and MPP under the second MH after MP application was correlated to subjective pain improvement. This study provides a strategy for the further design and application of MPs for metatarsalgia treatment.
[/contentbox]